A 35 year-old primigravida, with uncomplicated pregnancy, was admitted to the hospital for induction of labor at 41 weeks’ gestation. Ultrasonography suggested the presence of oligohydramnios. Fetal heart rate monitoring disclosed both late and variable decelerations. Induction of labor with oxytocin was successful. A 3700-g female infant is delivered and covered with meconium. The infant is limp with agonal respirations and a heart rate of 92.
Meconium aspiration is the inhalation of the first stool of a newborn, a thick, dark-green substance known as meconium. A fetus in distress in utero will often pass meconium in the amniotic fluid, and this is more likely to occur in infants who are term or post term (36->42 weeks gestation). Meconium aspiration usually results in early onset respiratory distress and has several deleterious mechanical, chemical and inflammatory effects on the respiratory system. 1

(http://www.mothering.com/forum/306-unassisted-childbirth/1063912-ucing-meconium-aspiration.html)
A mechanical effect is the obstruction of the airway with meconium, which could lead to atelectasis or hyperinflation. This may alter the ventilation to perfusion ratio or result in barotrauma. Normally, surface tension is reduced by the presence of surfactant. However, infants with meconium aspiration have an increase in surface tension due to the loss of a phospholipid substance, which forms surfactant. This chemical effect of surfactant inhibition mainly results in decrease in lung compliance. In addition, lung injury is caused by the release of the inflammatory mediators that lead to pneumonitis or epithelial airway injury.2
Research has found that prolonged labor, method of delivery, premature rupture of the membrane, presence of meconium on the infant, fetal distress and fetal asphyxia are all risk factors of developing meconium aspiration and respiratory distress.3 Signs and symptoms of infants with meconium aspiration include cyanosis, nasal flaring, retraction on inspection and grunting. Additionally, auscultation of the lungs may reveal crackles.4
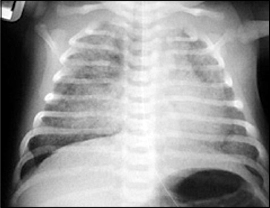
A variety of modalities and methods can be used in the diagnosis of meconium aspiration. One is through observation of the presence of meconium in the airways by visualizing the vocal cords. Blood gas abnormalities may indicate the development of respiratory distress due to meconium aspiration. Another modality that has played a significant role in the diagnosis of respiratory distress and meconium aspiration is the utilization of chest x-rays .5 Chest x-rays may reveal patchy infiltrates and hyper-inflated lungs, which are commonly seen in infants with meconium aspiration.6
http://www.adhb.govt.nz/newborn/TeachingResources/Radiology/LungParenchyma.htm#RDS
After the diagnosis of meconium aspiration has been confirmed, it is important to treat the patient as soon as possible to prevent any further complications. The treatment depends on the severity of illness and underlying cause. Suction of the meconium through bulb or suction catheter could be beneficial, but do not intubate the patient just for the sake of suctioning. One of the main treatments used for meconium aspiration is surfactant replacement therapy. Surfactant administration tends to reduce the need for supplemental oxygen, the duration of mechanical ventilation, the incidence of developing pneumothorax and the mortality rate. Another type of therapy used is high frequency oscillatory ventilation (HFOV). However, although it is widely used and has potential benefits, there is a lack of strong evidence supporting the use of HFOV over conventional mechanical ventilation. In very severe cases, infants may develop septic shock or experience cardiac complications. Extracorporeal membrane oxygenation (ECMO) therapy is generally used as a last resort in infants who would die without this form of therapy. Special precautions should be taken when dealing with infants suffering from neurological, nutritional, and musculoskeletal disorders because ECMO could have an effect on increasing morbidity.7

http://www.rosenfeldinjurylawyers.com/meconium-aspiration-syndrome.html
References:
1- Wiedemann, Jeanne R, et al. “Meconium aspiration syndrome.” Neonatal network 27.2 (2008):81-87. Web.
2- van Ierland, Y, and A J J de Beaufort. “Why does meconium cause meconium aspiration syndrome? Current concepts of MAS pathophysiology.” Early human development 85.10 (2009):617-620. Web.
3-Singh, S N, et al. “Respiratory distress including meconium aspiration syndrome in vigorous neonates born through meconium stained amniotic fluid: incidence, onset, severity and predictors at birth.” The Indian Journal of Pediatrics 80.7 (2013):538-543. Web.
4- Edmonds, Patricia. “An introduction to meconium.” Midwifery today with international midwife .111 (2014):32-33. Web.
5- Czarnecki, L M, and Łukasz M Czarnecki. “DIAGNOSTIC IMAGING Assessment of chest X-ray images in newborns with respiratory disorders.” Kardiochirurgia i Torakochirurgia Polska 12.1 (2015):83-86. Web.
6-1. Lynne M, Smith. Meconium Aspiration Imaging.retrived on Friday 04-16-2016 http://emedicine.medscape.com/article/410756-overview
7- Gortner, Ludwig. “Adjunctive therapies for treatment of severe respiratory failure in neonates.” Klinische Pädiatrie 227.2 (2015):51-53. Web.\\\\\\\\
